November 9, 2015
Via online submission to www.regulations.gov
Ms. Jocelyn Samuels
Director, Office for Civil Rights
U.S. Department of Health and Human Services
Attn: 1557 NPRM (RIN 0945-AA02)
Hubert H. Humphrey Building
200 Independence Avenue SW
Washington, DC 20201
Re: Affordable Care Act Section 1557 Notice of Proposed Rulemaking (RIN 0945-AA02)
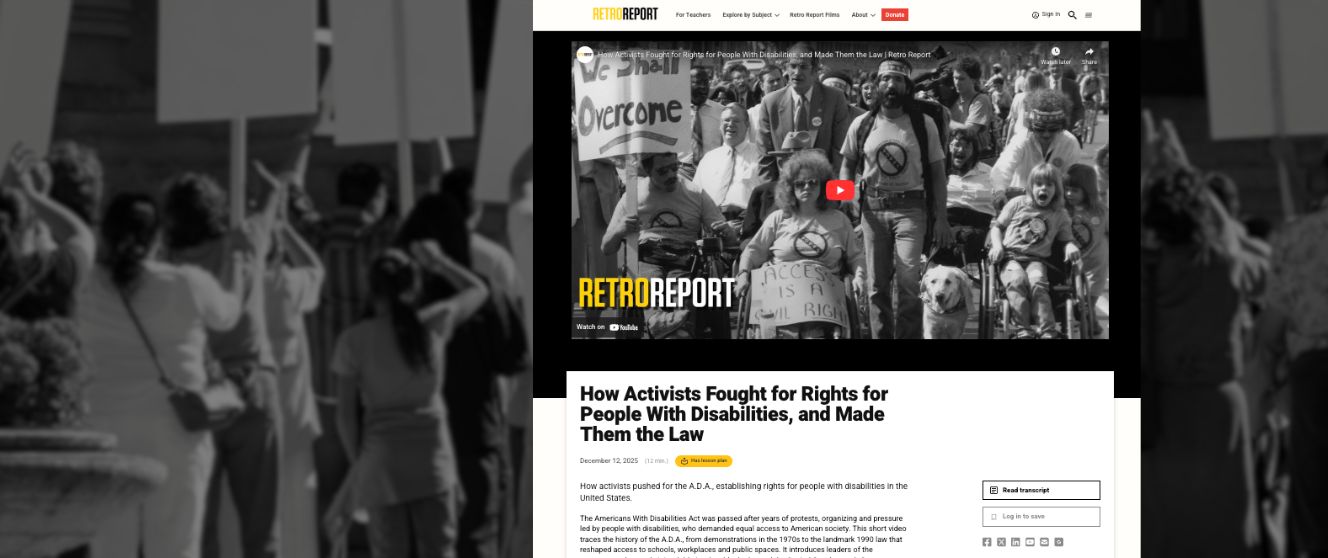
Disability Rights Education and Defense Fund (DREDF) appreciates the opportunity to provide comments on the above proposed rulemaking on Section 1557 of the Affordable Care Act (“1557 rule”). As an organization founded by people with disabilities and parents of children with disabilities, we acknowledge how much people with disabilities of all ages need effective, accessible healthcare in their communities. Even after the passage of Section 504 of the Rehabilitation Act of 1973 (Section 504) and the Americans with Disabilities Act of 1990 (ADA), the disability community has struggled with discrimination such as a lack of physical and programmatic accessibility, false stereotypes, and imbedded prejudice in healthcare delivery and health insurance design. The proposed 1557 rule is a necessary tool for achieving health care equity for people with disabilities.
Introduction
DREDF recognizes that the Health and Human Services’ Office of Civil Rights (HHS OCR) has taken a number of positive steps in the proposed 1557 rule to address discrimination in healthcare availability, design and delivery. In particular we applaud OCR’s efforts to prevent discrimination experienced by LGBT individuals who seek healthcare and marketplace participation. For persons with disabilities, the proposed rule takes the important step of identifying 1557’s application in a number of healthcare contexts. Many healthcare entities who may pay greater attention to HHS regulations and policy guidance than to what may appear to be distinct federal civil rights laws. The proposed rule nicely clarifies that existing Rehabilitation Act regulations governing such areas as physical and equipment accessibility, programmatic accessibility (modification of a covered entity’s policies, procedure and practices) and effective communication apply to all entities receiving federal financial assistance (FFA).
However, DREDF also believes that the current proposed rule fails to critically develop what disability non-discrimination would and should look like in the current US healthcare system under the Patient Protection and Affordable Care Act (ACA).. Limitations such as the historic exclusion of Part B providers are imported into the proposed rule almost by rote, while key opportunities to elaborate on how 1557 applies in the growing context of managed care delivery systems, provider network accessibility, benefit design, and the right to live in the community are overlooked. Finally there is little or no recognition of how discrimination can doubly impact those who have a disability and are also a member of another minority group that also experiences health disparities; we raise this because the accommodations needed by individuals in such situations may require thoughtful tailoring rather than an attempt to force a choice between personal characteristics.
Section by Section Comments
92.4 Definitions
Federal Financial Assistance — Part B Providers
We are very disappointed by the proposed rule’s ongoing exclusion of Medicare Part B providers from the definition of Federal Financial Assistance, and the extension of this exclusion to Section 1557.[1] The plain meaning of Section 1557’s text clearly includes Part B providers, and we believe that the prior HHS policy excluding Part B providers from compliance with Title VI is based on an antiquated definition of Federal Financial Assistance and should not be extended to Section 1557 (and indeed should be rescinded for Title VI).
In the context of Title VI, the exclusion of Part B providers arose soon after enactment of Medicare, based upon two rationales: (1) Medicare Part B was not a “contract of insurance,” and (2) Medicare Part B providers were not directly paid by the federal government so no federal financial assistance exists. In 2015, these two rationales cannot be reasonably applied to Section 1557.
i. Contract of Insurance Rationale
As one rationale for exclusion, HHS relied on Title VI’s statutory language excluding “contracts of insurance.” While we believe the original reliance on this exclusion was specious, the statutory language of Section 1557 specifically includes “contracts of insurance,” so this rationale cannot apply to Section 1557.
Title VI’s legislative history documents that inclusion of “other than contracts of insurance” in Title VI was “clearly designed to assure that programs or activities financed with loans from non-Federal sources were not subject to the prohibitions of the title merely because such loans were not federally insured.”[2] The legislative understanding was focused on a particular concern that Title VI — applicable to all federal financial assistance and not just health programs — should not apply to home mortgages obtained from federally insured institutions or deposits in federally insured banks. As Senator Humphrey, the Senate floor leader for the Civil Rights Act, stated:
The exclusion relates to, as the language says, other than a contract of insurance or guarantee. So FDIC (Federal Deposit Insurance Corporation) and all activities pertaining thereto are eliminated. The Federal Housing Administration is eliminated.[3]
Senator Pastore, Senate floor manager for Title VI, iterated this purpose of the exclusion:
The reason why we have excluded contracts of insurance or guaranty is that we do not want this section to affect, let us say, guarantees of deposits in banks . . . . We do not want that section to affect FHA housing. That is precisely why the exception is put in the section.[4]
All historical accounts point to an understanding that the section was limited to banking and housing and that Title VI did apply to federally assisted medical health care programs in existence at the time of its passage, let alone to Medicare at the time that program was enacted.[5] The specific inclusion of “contracts of insurance” in Section 1557 negates this as a rational explanation for excluding Part B providers.
ii. Direct Payment Rationale
According to an analysis by the U.S. Commission on Civil Rights, HHS’s original decision to exclude Part B providers was due in part to the HHS Office of General Counsel’s determination that Medicare Part B did not constitute Federal Financial Assistance because the reimbursement was paid directly to beneficiaries, not to health care providers, and was “limited to 80 percent of the reasonable costs.”[6] Even then, this reasoning was somewhat suspect since payments were only made to beneficiaries contingent upon their receipt of the health services Medicare was intended to provide.[7]
Regardless of past practice, Medicare today does provide direct payments, through Medicare Administrative Contractors, to providers with very few opting out of this “assignment” system. There are many markers of the direct contractual relationship between Part B providers, including individual physicians, and HHS’s Centers for Medicare and Medicaid Services (CMS). Part B providers must enroll in Medicare and, as part of that enrollment, certify that they will abide by all Medicare laws, regulations and program instructions applying to them, including federal civil rights laws.[8] They must comply with all applicable conditions of participation in Medicare. CMS imposes many direct obligations on enrolled providers. For example, they are limited in the amounts that they charge Medicare beneficiaries; they must provide Advanced Beneficiary Notices when appropriate; they are subject to balance billing prohibitions when serving Qualified Medicare Beneficiaries (QMBs). The notion that these enrolled providers, subject to multiple conditions for payment and multiple detailed requirements imposed by statute, regulation and sub-regulatory guidance, are merely getting payments passed on by beneficiaries is a fiction.
In any event, as HHS notes in the NPRM’s preamble, Title IX payments made either to a student or to an institution both count as Federal Financial Assistance:
This provision was included in the Title IX regulation to make clear that both funds paid to the educational entity on behalf of a student, and funds paid to the student and then remitted to the educational entity, are Federal financial assistance.[9]
The preamble likewise states that Advanced Premium Tax Credits (APTCs) and Cost Sharing Reductions (CSRs) — whether extended to the entity or to the individual for remittance — are Federal Financial Assistance.[10] Thus the explanation that Medicare Part B payments did not constitute federal financial assistance in the 1960s is not only factually unjustified today, it is outweighed — and indeed overridden — by subsequent changes in program structure and reimbursement as well as the contrary interpretation of student aid, APTCs and CSRs.
Given that we now operate under one unified statutory provision that prohibits discrimination on the basis of race, color and national origin, disability status, and sex, differing standards cannot continue when the result is that some individuals will be protected from nondiscrimination while others will not. When examined more closely, it is entirely arbitrary to base Section 1557 coverage distinctions on factors such as the type of program (e.g., Medicare or Medicaid), or on where care is physically received (e.g., a hospital ER or a local provider’s office). In the 60s, the HHS Office of General Counsel attached importance to the fact that Medicare payments were “limited to 80 percent of the reasonable costs.”[11] But today, other programs which HHS accepts as indisputable covered under Section 1557 — such as Medicaid and CHIP — likewise often do not pay providers 100 percent of their costs but rather lower, negotiated rates.
Similarly, HHS accepts that Part A providers such as hospitals, rural health clinics and federally qualified health centers are FFA recipients under Section 1557, yet a comparison of CMS’s dealings with Part A providers and Part B providers demonstrates that there is no reason to distinguish between the categories. Part A and Part B providers both must enroll in Medicare. Medicare Administrative Contractors (MACs) process both Part A and Part B claims. Both Part A and Part B providers have the right to themselves appeal Medicare coverage determinations; neither must rely on the beneficiary to initiate an appeal.[12] CMS has itself created a single provider bulletin for Part A & B providers about their appeal rights.[13] Part A and B providers both sign provisions within their Medicare contracts to honor federal civil rights law including section 504. Individuals with disabilities who are protected from discrimination when they seek care in a hospital emergency room department should get the same protection from discrimination and physical and programmatic accessibility when they seek earlier timely preventive care through a Part B provider. Any decision otherwise creates additional perverse incentives to low-income or homeless individuals to avoid ongoing preventive care until they have no option but to seek emergency room intervention.
iii. Impact on Consumers
The NPRM’s regulatory impact analysis concludes that very few health care providers only accept Medicare Part B and thus would be exempt from the proposed regulation. First of all, this analysis was limited to physicians and did not include other important healthcare providers such as Durable Medical Equipment providers, home health providers, non-physician mental and physical health therapists, and many other providers who people with disabilities in particular rely upon to maintain functional capacity and health. Secondly, there is no attempt to consider the possible profile of those individual Part B physicians who may not be caught under these other forms of FFA. Quite possibly these are small highly profitable specialty practices or partnerships that choose not to participate in Medicaid and also avoid the administrative complications of joining managed care provider networks. From the point of view of the consumer, and especially persons with disabilities who generally have a greater need for specialty care services, why should such practices have a lower standard to meet with regard to non-discrimination and ensuring accessibility and accommodation, regardless of the real number of such practices?
Ultimately, from the consumer’s point of view, there is no justification for not including all healthcare providers under Section 1557’s civil rights mandate, regardless of whether they receive Medicare, Medicaid, or any other form of FFA. Medicare consumers with disabilities should not have to hesitate before requesting an accommodation to ensure that the provider in question has another source of FFA, and OCR investigators should not have to trace through the entire stream of federal funding to a provider who discriminates on the basis of disability, race, ethnicity or sex. In DREDF’s experience, many consumers are initially unsure whether they have coverage under Medicare or Medicaid. If they are told that the OCR does not accept complaints against Medicare Part B providers because they are not subject to Section 1557, veryfew or no consumers will have the wherewithal to figure out if their provider actually receives some other form of FFA, especially if that consumer or their family member is in the midst of a health-related crisis.
Finally, very recent policy discussions have been initiated around the potential for including physical accessibility information in the online “Physician Compare” component of Medicare.gov. Comments on a Request for Information relating to the implementation of a Merit-based Incentive Payment System (MIPS) for physicians, enacted as part of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), raise new potential for incentivizing physical and programmatic accessibility among individual providers. The 1557 non-discrimination rule should support such policy efforts to gather critical data and increase accessibility for Medicare beneficiaries with disabilities, not perpetuate a harmful, discriminatory policy enacted in a prior era when it was wrongly regarded as legitimate for health care providers to exclude or provide unequal treatment to certain patients.[14]
As the U.S. Commission on Civil Rights concluded in 1980, Medicare Part B payments are clearly Federal Financial Assistance and should not be excluded from Title VI as either contracts of insurance or by reason of the method of their payment.[15] The passage of time, the change in Medicare payment methods and the specific inclusion of “contracts of insurance” in Section 1557 directly point to the need to correct the antiquated policy excluding Medicare Part B providers from FFA. In the alternative, if HHS cannot change its historical policy, the developments over the past twenty-five years as well as the statutory text of Section 1557 definitively demonstrate that Medicare Part B providers should at least be subject to compliance with Section 1557.
We strongly urge HHS to reverse its exclusion of Part B providers. All Medicare providers, without exception, should be subject to Section 1557’s civil rights mandates. Further, because including Part B providers would constitute a change in existing policy, we ask that HHS explicitly state, within the text of the regulation, that Part B provider payments constitute Federal financial assistance.
DREDF recommends amending the definition language of Section 92.4 as follows (suggested language in italics):
Federal financial assistance.
(1) Federal financial assistance means any grant, loan, credit, subsidy, contract (other than a procurement contract but including a contract of insurance), or any other arrangement by which the Federal government provides or otherwise makes available assistance in the form of: (i) Funds; (ii) Services of Federal personnel; or (iii) Real and personal property or any interest in or use of such property, including: (A) Transfers or leases of such property for less than fair market value or for reduced consideration; and (B) Proceeds from a subsequent transfer or lease of such property if the Federal share of its fair market value is not returned to the Federal government.
(2) Federal financial assistance provided or administered by the Department includes all tax credits under Title I of the ACA, as well as payments, subsidies, or other funds extended by the Department to any entity providing health insurance coverage for payment to or on behalf of an individual obtaining health insurance coverage from that entity or extended by the Department directly to such individual for payment to any entity providing health insurance coverage, including contracts for insurance, payments, subsidies, or other funds received directly or indirectly by Medicaid and Medicare providers, including Medicare Part B providers.
Federal Financial Assistance — Research Activities
DREDF continues to strongly advocate for the need for the explicit inclusion in the final rule of health care and health services research that receives FFA. These research activities must be included amongst the critical programs and activities that are considered health programs or activities under Section 1557, especially when much of this research in intended, implicitly or explicitly, to help establish standards for evidence-based treatment and prescription standards. The development of clinical research that does not involve PWD will lead to treatment standards that will ignore the needs of PWD.[16] As federally conducted or federally funded health programs or activities, all government supported research activity must encourage addressing disability-related issues and health disparities research in funded studies. Similarly all government support research activity, whether initiated under the ACA or not, must require including PWD within the study populations in the same way that members of other medically vulnerable or underserved groups, such as women or racial minorities, are required for inclusion. Research proposals that explicitly, or by design, fail to address the recruitment of PWD must explain the rationale or medical value of such an exclusion.[17] Scholarships, grants, and tuition waivers/reimbursement incentives must be provided to researchers and scholars who pursue disability-related research topics in the same way, for example, that the National Institutes of Health provide such incentives to minority researchers. In the current landscape, researchers with disabilities that seek to perform disability-related health research face an unequal playing field when they pursue funding opportunities.
The Department misunderstands the impact of including healthcare research within FFA when it states that “For example, a medical research institution that is a covered entity may exclude individuals who are a deaf from a clinical trial to investigate a new brain imaging technology for assessing cognitive functioning that relies on auditory stimulation as the test stimulus. This research design would not be discriminatory on the basis of disability because there is a nondiscriminatory justification for excluding individuals who are deaf.” We understand that such a research trial would not be discriminatory for excluding Deaf persons. But it would be discriminatory to exclude Deaf persons from myriad other kinds of clinical trials and research simply because the investigators did not want to incur the expense of sign language interpreters. The final rule needs to clarify this distinction, rather than leave the impression that clinical researchers are free to consider “cost” as a non-discriminatory factor in trial design. Participation in research and clinical trials is not necessarily for the benefit of individual participants, but participants without disabilities have the freedom, choice and responsibility to engage in such research for the benefit of those similarly situated. That same choice and responsibility must be extended to people with disabilities.
92.101 Discrimination Prohibited
Section 92.101(b)(2)(i) incorporates regulations enacted under Section 504 that pertain to recipients of federal financial assistance, extending these regulations to include State-based marketplaces. In general we support OCR’s aim in paragraphs (b)(1-4) to “incorporate into this proposed regulation the specific discriminatory actions prohibited under each civil rights law on which Section 1557 is grounded.”[18] We think this approach is preferable given the ambit and breadth of private health care entities that are subject to Section 1557 through their participation in federal and state marketplaces. These entities may not be readily familiar with specific regulatory standards and obligations under Section 504 and the Americans with Disabilities Act of 1990 (ADA) that now apply to them. We also agree that explicit incorporation will help avoid “confusion and unintended consequences in interpretation between the different federal civil rights laws that Section 1557 references.
At the same time, the incorporation of existing Section 504 and ADA regulations must be done carefully and in a manner that will not unnecessarily narrow the ambit of Section 1557 in its intended governance of existing and newly covered entities in the healthcare context. In particular, we object to the application of all of Section 504’s program accessibility provisions for existing facilities, 45 CFR §§.84.22 and 85.42, to the many health insurance issuers and managed care organizations that operate health programs and activities in state marketplaces and Medicaid programs, in Medicare, and in the federal marketplaces.
First of all, the same “confusion and unintended consequences” that OCR foresees in an attempted harmonization of regulatory standards and concepts between civil rights statutes is potentially raised by the failure to harmonize regulatory standards and concepts within Section 504’s cited regulations. 45 CFR §§.84.22 and 85.42 differ slightly in their language, but there is no principled reasons that State-based Marketplaces and Federally-facilitated Marketplaces should apply program accessibility in existing facilities in slightly different ways. Each type of marketplace, for example, should have the same obligation to make existing facilities readily accessible to and useable by persons with disabilities unless it can establish a fundamental alteration or undue burden defense. State and municipal entities are, of course, already familiar with that concept under Title II of the ADA and 28 CFR § 35.150, but 45 CFR §.84.22 does not contain this actual language.
Second, both §§.84.22 and 85.42 incorporate a concept of “program accessibility” that was developed specifically for government programs and agencies. The concept allowed government programs to assess the physical accessibility of a program or activity “in its entirety” given that many traditional federal and federally funded operations took place in older buildings and locations that could be especially burdensome to modify in every instance. Decades after passage of Section 504, program accessibility is highly inappropriate in the context of private insurance carriers and managed care organizations that encompass literally hundreds or thousands of distinct providers within their “health program or activity.” A key feature of how these large corporate entities appeal to prospective members is through the quality, size and “choice” offered within each entity’s provider networks. At the same time, state insurance and Medicaid agencies and the Centers for Medicare and Medicaid Services work to establish clear guidelines and consumer protections to govern the sufficiency of provider networks. Amidst this backdrop of private competition and regulatory practice, it would be senseless to allow private entities to essentially decide for themselves when their provider network is “readily accessible” to people with disabilities. Yet, that is exactly what will happen if such private entities are subject to a program accessibility standard that “does not require a recipient to make each of its existing facilities or every part of a facility” accessible to and useable by persons with disabilities. The clear implication is that a large for-profit insurance carrier could decide that, among the great majority of its providers who operate in existing facilities, only 10% or some other arbitrary percentage need to be physically accessible or have accessible equipment. Moreover those accessible providers could be clustered together in some central location, and whenever a member calls member services and mentions the need for accessibility, that member will be actively directed toward “the accessible provider offices.”
As written and potentially applied, §§.84.22 and 85.42 could gut the concept of provider choice for health consumers with disabilities, and also conflict with state and federal regulations that place provider time and distance or provider-member ratio obligations on insurance carrier and managed care provider networks. Or perhaps provider network regulations are met on paper, but there will be a real life scarcity of accessible providers who are actually willing and able to take new members with disabilities. While the general prohibition of discrimination in s. 92.101(5) of the proposed rule is supposed to take primacy over the specific forms of discrimination enumerated in s. 92.101(2)(b)(i) and (ii), the full incorporation of the program accessibility concept will give covered entities an unintended escape hatch that relegates health consumers with disabilities to second-place status every time they try to gain access to their provider network. The fact is, every healthcare provider is already independently subject to Title III of the ADA, and as a recipient of federal financial assistance under Section 1557, is responsible for ensuring that the “entirety” of its program or activity is readily accessible to and useable by persons with disabilities. These individual providers may not have multiple locations and existing facilities to pick and choose among for “program accessibility purposes. It would surely be an unintended consequence if corporate insurance entities that establish extensive provider networks could, by that very fact, escape using their greater resources and administrative capacity to facilitate increased accessibility among those same providers.
In light of the above, we recommend that the Department adopt regulations under Section 92.101 that harmonize 45 CFR §§.84.22 and 85.42 primarily though the amended language of § 85.42 as follows (suggested amendments in strike-out):
§ 85.42 Program accessibility: Existing facilities.
(a) General. The agency shall operate each program or activity so that the program or activity, when viewed in its entirety, is readily accessible to and usable by individuals with handicaps. This paragraph does not—
(1) Necessarily require the agency to make each of its existing facilities accessible to and usable by individuals with handicaps; or
(2) Require the agency to take any action that it can demonstrate would result in a fundamental alteration in the nature of a program or activity or in undue financial and administrative burdens. In those circumstances where agency personnel believe that the proposed action would fundamentally alter the program or activity or would result in undue financial and administrative burdens, the agency has the burden of proving that compliance with§ 85.42(a) would result in such alteration or burdens. The decision that compliance would result in such alteration or burdens must be made by the agency head or his or her designee after considering all agency resources available for use in the funding and operation of the conducted program or activity in question, and must be accompanied by a written statement of reasons for reaching that conclusion. If an action would result in such an alteration or such burdens, the agency shall take any other action that would not result in such an alteration or such burdens but would nevertheless ensure that individuals with handicaps receive the benefits and services of the program or activity.
(b) Methods.
(1) The agency may comply with the requirements of this section through such means as redesign of equipment, reassignment of services to accessible buildings, assignment of aides to beneficiaries, home visits, delivery of services at alternate accessible sites, alteration of existing facilities and construction of new facilities, use of accessible rolling stock, or any other methods that result in making its programs or activities readily accessible to and usable by individuals with handicaps. The agency is not required to make structural changes in existing facilities where other methods are effective in achieving compliance with this section. The agency, in making alterations to existing buildings, shall meet accessibility requirements to the extent compelled by the Architectural Barriers Act of 1968, as amended (42 U.S.C.
4151-4157), and any regulations implementing it.
(2) In choosing among available methods for meeting the requirements of this section, the agency shall give priority to those methods that offer programs and activities to qualified individuals with handicaps in the most integrated setting appropriate.
(c) Time period for compliance. The agency shall comply with the obligations established under this section within 60 days of the effective date of this part except where structural changes in facilities are undertaken; such changes shall be made within three years of the effective date of this part, but, in any event, as expeditiously as possible.
(d) Transition plan. In the event that structural changes to facilities must be undertaken to achieve program accessibility, and it is not expected that such changes can be completed within six months, the agency shall develop, within six months of the effective date of this part, a transition plan setting forth the steps necessary to complete such changes. The agency shall provide an opportunity to interested persons, including individuals with handicaps or organizations representing individuals with handicaps, to participate in the development of the transition plan by submitting comments (both oral and written). A copy of the transition plan shall be made available for public inspection. The plan shall, at a minimum—
(1) Identify physical obstacles in the agency’s facilities that limit the accessibility of its programs or activities to individuals with handicaps;
(2) Describe in detail the methods that will be used to make the facilities accessible;
(3) Specify the schedule for taking the steps necessary to achieve compliance with this section and, if the time period of the transition plan is longer than one year, identify steps that will be taken during each year of the transition period; and
(4) Indicate the official responsible for the implementation of the plan.
Please note: We have incorporated comments regarding 92.101(b)(2)(i)’s discussion of 45 CFR 84.23(c) and the Uniform Federal Accessibility Standards (UFAS) in our section on 92.203 on Accessibility Standards for Buildings and Facilities.
92.101(b)(2)(ii) — specific prohibition of discrimination on the basis of disability for the Department and Federally Facilitated Marketplaces.
See above comments on 92.101(b((2)(i).
92.203 Accessibility Standards for Buildings and Facilities
We support OCR’s position in the draft rule to adopt the 2010 ADA Standards for Accessible Design (2010
Standards) as the relevant standard required in any facility or part of a facility in which health programs or activities are conducted that is constructed or altered by or on behalf of, or for the use of, a recipient or State-based marketplace. We agree with OCR’s observation at 80 FR 541i6 that “nearly all of the facilities covered under the proposed rule are already subject to the 2010 Standards.” As a result, we are uncertain why the proposed rule gives new construction and alteration an additional time period to come into compliance with the 2010 Standards. That is, the proposed rule applies the 2010 standards to new construction and alteration that is commenced 18 months after publication of the final 1557 rule. However, the 2010 Standards themselves applied to newly constructed State and local government facilities if they were constructed on or after March 15, 2012. The vast majority of facilities covered by this proposed rule were already subject to the 2010 standards as of March 15, 2012. We do not think there needs to be another “safe harbor” period for facilities in which health programs or activities are conducted that are newly constructed or altered between March 15, 2012 and a date that is 18 months after publication of the final 1557 rule.
We recognize that there may be some ADA Title III entities participating in the federal or state marketplaces that arguably did not yet know that specific new construction or alteration standards would apply to them under s. 1557 absent OCR’s proposed rule language. Such new construction or alteration would in any event have fallen under Appendix A of the 1991 Title III regulation, which is republished as Appendix D to 28 CFR part 36, containing the ADA Standards for Accessible Design (1991 Standards). We would therefore support, if this were found to be necessary, the tailored recognition that such facilities, where construction or alterations were commenced before 18 months from the final date of the rule, are deemed to comply with the requirements of this proposed rule and with 45 CFR 84.23 (a) and (b), cross referenced in § 92.101(b)(2)(i) with respect to those facilities, if they are in conformance with the 1991 Standards or the 2010 Standards.
An approach which emphasizes the uniform application of the 2010 Standards upon publication of s. 1557 rule will enable greater consistency among implementing agencies, given the overlapping jurisdiction that OCR has with the Department of Justice, which will apply the 2010 Standards to Title II facilities constructed or altered after March 15, 2012. Complainants with disabilities should not be implicitly influenced toward one administrative forum or another by the date on which a healthcare facility’s construction or alteration began. More substantively, the 2010 Standards have specific provisions that apply to “Medical care facilities” which recognize the importance of having accessible patient bedrooms in all areas of a facility in order to facilitate access to needed medical specialty providers and equipment by people with disabilities. Such specificity makes the 2010 Standards especially appropriate for the widest possible adoption in the s. 1557 regulations.
Under a similar rationale, we strongly agree with OCR’s decision in 92.101(b)(2)(i), with respect to existing facilities, to not adopt “the program accessibility provision at [45 CFR] § 84.23(c), addressing conformance with the Uniform Federal Accessibility Standards for the construction and alteration of facilities, because these standards are outdated.” We do not, however, understand or agree with the ongoing incorporation of the Uniform Federal Accessibility Standards (UFAS) in s. 92.203(b), which states that compliance with UFAS shall be deemed to be compliance with s. 1557 for newly constructed or altered facilities “if the construction or alteration was commenced before [18 MONTHS FROM DATE OF PUBLICATION OF FINAL RULE].”
We object to the ongoing incorporation of UFAS not on superficial stylistic grounds, but because UFAS is
functionally deficient for people with disabilities. Accessibility barriers are permitted under the old standard that particularly affect people with mobility and strength disabilities. In November 2007, the Department of Veteran Affairs (VA) issued A Barrier Free Design Guide: A Supplement to the Uniform Federal Accessibility Standards.[19] The purpose of the guide was to tailor UFAS requirements so that health care facilities, in particular, would meet the barrier free needs of the Department of Veterans Affairs (VA). A quick glance at the footnotes of the guide reveal the extent to which UFAS standards fall short of ensuring accessibility for people with disabilities:
4. The disabled population used by UFAS to determine an acceptable slope for using public accommodations
is stronger and younger than are veterans at VA facilities.
5. UFAS used a younger, more fit population to determine the minimum slope and distance for a disabled
person’s travel capability.
7. UFAS is based on an active, independent population. Little consideration was given to accessibility
in medical care facilities, except in Section 6.[20]
12. Tests show only those with good upper body strength can manage a ramp slope of 1:12. Slopes greater
than 1:16 create safety hazards for any wheeled vehicle.
20. Window sills must be low enough that seated (wheelchair) and bedridden patients can see outside.
24. The UFAS 900 mm x 900 mm (3′-0″ x 3′-0″) shower has a folding seat which requires the patient to
transfer from the wheelchair. The UFAS 750 mm x 1500 mm (2′-6″ x 5′-0″) shower admits a wheelchair, but just barely. There is no room for the patient to maneuver or for attendants to help.
The VA website currently states that it:
follows GSA [the General Services Administration] and other standard-setting agencies in replacing UFAS with the Architectural Barriers Act Accessibility Standard (ABAAS) for Federal Facilities. In addition, VA uses the Barrier Free Design Guide to meet the needs of the Department of Veterans Affairs in its health care facilities.it has officially adopted the 2010 Standards in place of UFAS.[21]
The VA and other federal agencies were able to replace the UFAS as the relevant standard for recipients of federal financial assistance because of actions taken by the Department of Justice. In a March 29, 2011 memo written by then Assistant Attorney General, Thomas Perez, to Federal Agency Civil Rights Directors, he noted that:
“several federal agencies have asked the Department, pursuant to its coordination authority for Section 504 under Executive Order 12250, if they have the authority to allow their recipients of federal financial assistance to use the 2010 Standards in lieu of UFAS. These agencies recognize that most of their recipients of federal financial assistance are also subject to the ADA and wish to minimize covered entities’ need to comply with multiple accessibility standards. In addition, many covered entities would prefer to use the 2010 Standards because they are written using language that is more consistent with the language used in many state building codes.”
In light of the above, the OCR’s retention of the UFAS standards for recipients and State-based Marketplaces appears to reward those few construction or alteration projects that did not have the foresight to take account of the needs of healthcare consumers with disabilities. The proposed rule, after all, only addresses facilities in which health programs or activities are conducted, not for example, a General Services or US Post Office building primarily intended for housing machinery.
Ultimately, with regard to disability, this rule reflects OCR, and more broadly the Department of Health and Human Services’ commitment to ensuring the accessibility to people with disabilities of federally funded healthcare programs and activities.. OCR and HHS overall should provide technical assistance to assist those few covered entities conducting health programs and activities in UFAS-only compliant facilities to come into compliance with the 2010 or 1991 Standards.
Medical Diagnostic Equipment
Overall, we support OCR’s plan to incorporate and enforce the Access Board’s standards for accessible medical examination and diagnostic equipment. We, too, eagerly await the release of final standards from the U.S. Access Board. However, DREDF is deeply aware of the degree to which the common lack of such equipment presents grave barriers to effective healthcare for people with mobility, strength and other disabilities.[22] It is difficult to assess when the U.S. Access Board will actually produce final standards, and even more difficult to assess whether and how scoping will be incorporated into the standards when they are eventually promulgated as regulations.
Given the prominence that the final rule will have among covered healthcare entities, we recommend that section 92.203 incorporate a subsection that explicitly requires “Each facility or part of a facility in which health programs or activities are conducted shall acquire accessible medical and diagnostic equipment as the program or activity engages in the purchase of new or additional equipment.”
Such a general direction will enable the Department to readily incorporate the more specific standards that are anticipate from the Access Board, while making it clear that covered are under an existing obligation to meet the physical and programmatic accessibility needs of people with disabilities. The interim obligation does not require any covered entity to expend resources on the immediate replacement of existing equipment with new equipment that may or may not meet the final Access Board standards, but it should at least initiate a slow and steady turnover from wholly inaccessible equipment to accessible exam tables, scales and other basic accessible equipment. This suggestion will also allow consumers with accessible equipment needs to have some degree of leverage in their current attempts to get providers to acquire accessible equipment. As currently written the proposed 1557 rule gives a person with disabilities little or no leverage, even if a provider, clinic or facility decides to run out and purchase the latest models of inaccessible equipment to replace medical equipment that had previously been accessible to some degree. The suggested wording will also enable OCR to more effectively enforce existing anti-discrimination laws and access standards whenever an individual with a disability is denied medical services because of the physical inaccessibility of the equipment. For practical enforcement purposes, OCR could use the Access Board’s Advisory Committee Report and Proposed Standards as guidelines until the final standards are issued.
92.204 Accessibility of Electronic Information Technology
We are appreciative of HHS’s unequivocal recognition that health-related information and technology must be accessible to and usable by people with disabilities in order to ensure effective and nondiscriminatory provision of health care services, and we strongly support HHS’s inclusion of explicit requirements in the proposed rule for accessible websites and electronic and information technology (E&IT). While it is true that Titles II and III of the Americans with Disabilities Act (ADA) and sections 504 and 508 of the Rehabilitation Act already provide both strong legal protections for consumers and a wealth of clear guidance for covered entities, we agree with HHS’s assessment that an express recapitulation of the general requirement to ensure accessible E&IT and websites is a critical regulatory reaffirmation which should, in the most effective and unmistakable manner possible, raise the profile of the need for dramatically greater compliance with current law.
We commend HHS for proposing to apply the nondiscrimination requirements to all of a covered entity’s E&IT and not to restrict the obligations only to websites or to specific classes or categories of E&IT. All too often, covered entities apply a piecemeal approach to ensuring that consumers of health information with disabilities do in fact have full and equal benefit from their services, programs and activities. Far too frequently, if access is provided at all, it is limited to a given context, such as accessible informed consent forms, and there is an utter lack of appreciation for the need to provide access at every stage of service delivery where all consumers are expected or invited to interact with online information or specific pieces of equipment. It is essential that covered entities understand that failing to afford access to consumers with disabilities at every stage of service delivery—from appointment setting, to in-person check-in, to interaction with any and all devices with which a covered entity expects consumers to use both in the in-patient and out-patient contexts, to review of medical records, billing and insurance data—not only discriminates against people with disabilities; such failure puts patients at tremendous risk inasmuch as the patient (or family member of a patient) with disabilities who is denied the ability to be a full and informed participant in his/her health care cannot be expected to fully understand diagnosis and treatment, to make informed choices about health care providers, or to respond appropriately to specific interventions. The risk extends to the consumer’s ability to maintain health coverage and needed benefits, or even choose an appropriate health plan in the first place, since billing and procedural coding errors cannot be timely reviewed when billing statements, summary notices, and summary of benefits documents are all too often partially or fully inaccessible, even when provided in an electronic format.
In addition to addressing the range of needs of consumers with disabilities, we anticipate that the proposal to cover all of a covered entity’s E&IT will assist healthcare professionals with disabilities to achieve greater independence and functional capacity as they exercise their profession. We know of numerous examples where people with disabilities in professions ranging from medical stenographer to licensed psychologists face additional E&IT barriers after they have already undergone rigorous training, educational and testing regimens because a hospital or managed care organization’s provider note and record systems are inaccessible to speech-reading software, for example. There is no principled reason for any aspect of a covered entity’s E&IT systems to be designed or maintained in a manner that cannot interface with the range of functional human capacities affecting vision, hearing, and speed and range of motion; this holds true for E&IT regardless of whether it is intended primarily or incidentally for public use. We strongly support the proposed rule’s requirement that all aspects of a covered entity’s E&IT be fully accessible. We also note that training, employing and retaining healthcare professionals with disabilities is a key means of reducing the widely recognized healthcare disparities experienced by people with disabilities.[23]
We believe that it would be useful for HHS to publish a final rule that is accompanied, in the preamble and/or explanatory notes, by illustrative examples of the various stages of health care delivery wherein online and E&IT means employed by covered entities need to be accessible. While we support the proposed text of section 92.204(a), we believe that a non-exhaustive set of examples would reinforce HHS’s intent to ensure applicability of these nondiscrimination requirements to all points at which covered entities use technology both now and in the future.
Given that proposed section 92.204 builds on and reinforces the other longstanding accessibility expectations of federal law, we strongly urge HHS to reject any application of a phase-in approach to these requirements. Just as HHS’s failure to include section 92.204 in its entirety in the final rule would not in any way diminish or impair the existing accessibility requirements that already apply to proposed Part 92-covered entities, HHS cannot and should not craft exceptions or limitations that are not otherwise in place. We believe that the existing undue burden and fundamental alteration analyses provide, as they have always provided, safeguards for covered entities and a proper balance between entities’ ability to comply and the rights of individuals with disabilities. We do, however, recommend that 92.204 include some explicit reference to the effective communication regulations that remain the legal origin point for the obligation to make websites and E&IT technology accessible. While not all of the regulations concerning auxiliary aids and services applies to the E&IT and website context, some are appropriate to incorporate. For example, where a covered entity may give sighted members the option to receive notices through email, a website portal, or electronic CDs, the covered entity may not impose only one of those options upon a member who is blind or visually impaired simply because that option is more convenient for the entity. The explicit incorporation of relevant aspects of 35 CFR §35.160(b)(2) informs covered entity’s that they must consult and work with members with disabilities as part of the entity’s effective communication obligation.
The following suggested language, in italics, for Section 92.204(b) encapsulates the above recommendations:
(a) Covered entities shall ensure that their health programs or activities provided through electronic and information technology are accessible to individuals with disabilities, unless doing so would result in undue financial and administrative burdens or a fundamental alteration in the nature of the health programs or activities. When undue financial and administrative burdens or a fundamental alteration exist, the covered entity shall provide information in a format other than an electronic format that would not result in such undue financial and administrative burdens or a fundamental alteration but would ensure, to the maximum extent possible, that individuals with disabilities receive the benefits or services of the health program or activity that are provided through electronic and information technology. In determining what types of electronic and information technology are necessary, a public entity shall give primary consideration to the requests of individuals with disabilities. In order to be effective, electronic and information technology must be provided in a timely manner, and in such a way as to protect the privacy and independence of the individual with a disability.
(b) State-based Marketplaces and recipients shall ensure that their health programs and activities provided through Web sites comply with the requirements of Title II of the ADA in accordance with the standards found at 28 CFR 35.160(a)(1) and (2), 35.160(d), 35.163, and 35.164. Where the regulatory provisions referenced in this section use the term “public entity,” the term “covered entity” shall apply in its place.
With respect to the application of ADA Title II or Title III standards to Part 92-covered entities’ website obligations, we recommend that the proposed rule require that E&IT comply with a specific set of standards such as Section 508 by the Access Board at 36 CFR part 1194 (Section 508 Standards), or the Worldwide Web Consortium’s Web Accessibility Initiative’s WCAG 2.0 AA (WCAG Standards). While we appreciate that Section 508 regulations are hopefully being finalized, we think it is important in this proposed rule to reaffirm the rights of people with disabilities, and redress current violations that occur when people with disabilities are given E&IT that fails to meet existing, readily available, and widely accepted standards.
This approach would have the benefit of clarity and consistency, and greater specificity will assist OCR in actual enforcement of the section. It will clearly inform OCR investigators that E&IT that falls short of the 504 or WCAG Standards falls within OCR’s jurisdiction and their authority to require correction from covered entities. We appreciate that covered entities will and should continue to engage in an interactive process on how to make E&IT fully accessible to individual consumers and employees, but it will be much more efficient to have compliance with the Section 508 or WCAG standards as the starting point in that discussion. The fact that DOJ is applying WCAG standards in its own Title II and III settlements supports our position that OCR should also adopt the 508 and WCAG Standards as interim standards before final Section 508 regulations are issued. To the extent that there is overlap between the Section 508/WCAG Standards and the Section 508 regulations, and such overlap is likely to be substantial, covered entities will be encouraged to take a head start towards what will eventually be required compliance with the Section 508 regulations.
This approach still leaves room for the expected evolution of E&IT requirements. Even the way in which we talk about categories of technology today, both domestically and internationally, is evolving; the term E&IT has itself fallen out of favor in the policy and other contexts in favor of the term information and communications technology (ICT). We therefore support HHS allowing this evolution to occur while providing, through the interim adoption of Section 508and WCAG Standards, a specific and currently enforceable statement of law that can only help to improve the full and equal participation of people with disabilities in America’s health care marketplace.
92.205 Requirements to Make Reasonable Modifications
We are pleased to see the requirements to make reasonable modifications for individuals with disabilities as proposed and agree that the language is consistent with the ADA. However, we believe this section needs to be strengthened through additional, clarifying language and healthcare-specific examples that will enable covered entities to understand the potential breadth and scope of the actions that can constitute a reasonable modifications. For example, the regulation should be clear that modifications to add medically necessary care for individuals with disabilities, or eliminating exclusions of medically necessary services, do not automatically constitute fundamental alterations to the nature of the health program or activity.
In addition, we also recommend that HHS provides specific examples of programmatic modifications that may be needed by individuals with disabilities. Such examples should include:
- Extended appointment times for individuals with disabilities that affect the speed and clarity of their communication or who use communication devices;
- Coverage of anesthesia for dental services when necessary for an individual with a disability to access dental or other medical care;
- Assistance with dressing or undressing;
- Putting appointment systems into place that will ensure that accessible examination rooms and/or equipment are available for the use of those individuals with disabilities who need them and
- Modification of wait times, office hours, and other business practices that may not be accessible for individuals with disabilities.
DREDF has done extensive work in this area and further examples of programmatic access are available on
our website at: https://dredf.org/public-policy/health-access-to-care-old/defining-programmatic-access-to-healthcare-for-people-with-disabilities/
92.207 Nondiscrimination in Health-Related Insurance and other Health-Related Coverage
§92.207(b) states in very general terms that plans shall not “deny or limit coverage of a claim, or impose additional cost sharing or other limitations or restrictions, on the basis of an enrollee’s or prospective enrollee’s race, color, national origin, sex, age, or disability; [or] (2) Employ marketing practices or benefit designs that discriminate on the basis of race, color, national origin, sex, age, or disability in a health-related insurance plan or policy, or other health-related coverage.” DREDF agrees wth the overarching goal of this requirement, but strongly recommend greater specificity in principle and through examples.
We urge the Department to provide additional guidance in the final rule concerning what constitutes
disability-based discrimination in health insurance, including discriminatory benefit design, discriminatory payment structures, discriminatory network design, and discriminatory coverage decisions. The bare statement in the proposed rule that Section 1557 prohibits discriminatory benefit design offers no information to beneficiaries about their rights under Section 1557 and no information to plan administrators, Medicaid officials, and others about their obligations under Section 1557. In order for Section 1557 to be implemented effectively, covered entities and protected individuals must have more guidance concerning the meaning of disability-based discrimination in health insurance.
This additional guidance is crucial because insurance companies have historically discriminated against people with disabilities in a wide variety of ways, and continue to do so, including through drug formularies, narrow networks, increased cost-sharing, wellness programs, utilization management programs, and limits or caps on certain services. These discriminatory practices are often driven by a desire to reduce costs. However, limiting access to health care for people with disabilities or chronic conditions is pennywise and pound foolish, often resulting in further complications and avoidable hospital admissions and readmissions.
We urge HHS to adopt the following principles in the final rule:
(i) Coverage that Promotes Needless Segregation
One form of disability-based discrimination is the needless segregation of individuals with disabilities. Olmstead v. L.C., 527 U.S. 581 (1999). See also 28 C.F.R. §35.130(b)(7) (covered entities shall administer services to individuals with disabilities in the most integrated setting appropriate to their needs). The Americans with Disabilities Act and Section 504 of the Rehabilitation Act require covered entities to serve individuals with disabilities in integrated settings unless doing so would “fundamentally alter” their service systems. HHS has recognized in the context of Medicaid managed care that insurance plans must comply with the ADA’s integration mandate, including having payment structures that encourage community-based care and benefits coverage that does not promote segregation.[24] Section 1557 explicitly incorporates Section 504’s prohibitions against disability-based discrimination. Hence disability-based discrimination under Section 1557 necessarily includes needless segregation just as it does under Title II of the ADA and Section 504.
To give effect to Section 1557, OCR should state clearly in the text of the final rule that discrimination under Section 1557 includes, among other forms of discrimination:
(a) Making coverage decisions that result in people with disabilities being served needlessly in segregated settings. For example, failure to cover services essential for people with psychiatric disabilities to live in their own homes or in supportive housing would violate the non-discrimination provision if it results in individuals being served in segregated settings such as hospitals, nursing homes, or board and care homes and covering the services to support them in integrated settings would not be unduly expensive.
(b) Setting reimbursement rates for coverage in a way that results in individuals with disabilities being served needlessly in segregated settings. For example, states cannot set reimbursement rates for services (including medications) in segregated settings (such as hospitals) higher than rates for similar services
in integrated settings.
(c)Designing a particular benefit — such as personal care services — so that it is offered in greater amounts to individuals in segregated settings.
(d)Placing maximum costs on Medicaid waiver services that fall below what it would actually cost to care for the individual in an institutional setting (and therefore extending beyond federally-required cost neutrality).
(ii) Unequal Coverage
OCR should state clearly in the text of the final rule that discrimination under Section 1557 includes, among other forms of discrimination:
(a) Failing to offer coverage that is as effective for individuals with disabilities as for individuals without disabilities — and similarly, failing to offer coverage that is as effective for individuals with a particular type of disability as for individuals with other types of disabilities.[25] Cf. 28 CFR §35.130(iii) (covered entities under Title II of the ADA shall not provide a qualified individual with a disability with an aid, benefit, or service that is not as effective in affording equal opportunity to obtain the same result, to gain the same benefit, or to reach the same level of achievement as that provided to others). For example, a plan that fails to cover core services commonly needed by people with HIV, or by people with intellectual or psychiatric disabilities, would violate Section 1557. Similarly, failure to cover durable medical equipment and assistive technology commonly used by individuals with physical disabilities would violate Section 1557. In addition, an insurance plan that covers organ transplants for most people but refuses to cover organ transplants for people with certain disabilities, based on stereotypes about people with disabilities and not on the likelihood that the transplant would provide a medical benefit, would violate Section 1557.
(iii) Disability-based coverage distinctions that are not justified by actuarial data.
OCR should clearly state in the text of the final rule that, in addition to other forms of discrimination, Section 1557 prohibits:
(a) Making disability-based distinctions in coverage that are not justified by legitimate actuarial data. Section 504 extends to the terms and conditions of insurance policies, and not simply to whether or not an individual is afforded insurance coverage. See, e.g., 28 C.F.R. Part 36, App. B, § 36.212 (Department of Justice regulations implementing Title III of the ADA, stating that “[l]anguage in the [ADA] committee reports indicates that Congress intended to reach insurance practices by prohibiting differential treatment of individuals with disabilities in insurance offered by public accommodations unless the differences are justified;” 29 C.F.R. Part 1630, App., § 1630.16(f) (EEOC interpretive guidance for regulations implementing Title I of the ADA, stating that a covered entity cannot deny a qualified individual with a disability equal access to insurance or subject a qualified individual with a disability to different terms or conditions of insurance based on disability alone if the disability does not pose increased risks). Section 504 prohibits all disability-based distinctions in insurance coverage that are not justified by legitimate actuarial data or actual or reasonably anticipated experience. 29 C.F.R. Part 1630, App., § 1630.16(f). Such data or experience cannot be based on generalized information about the cost of covering individuals with a particular condition or covering particular services, and must be consistent with the ACA’s community rating provisions.
Additional Examples of Disability Discrimination in Benefit Design
The disability community included many examples of disability discrimination in health programs and activities in response to the RFI and we would refer OCR back to those comments.[26] In addition, DREDF wishes to provide OCR with additional specific examples of disability-based discrimination, which we urge OCR to include in the final rule:
(i) Organ Transplants
An example of a “health care program or activity” in which people are regularly discriminated against today on the basis of disability alone, rather than on the efficacy of the treatment, is organ transplantation. People disabilities — particularly people with intellectual disabilities and developmental disabilities — are regularly denied access to organ transplants on the basis of their disability. According to multiple studies conducted on organ transplant centers in the United States, many centers consider the mere presence of intellectual or developmental disability to be a contraindication to transplantation.[27] This was more likely to be true of heart transplants than other transplants.[28] Ironically, heart transplants are of critical utility to people who also have co-occurring congenital heart conditions, such as those that often occur in Down Syndrome.[29]
While this form of discrimination is prohibited under federal anti-discrimination provisions (such as the ADA and Section 504 of the Rehabilitation Act), there is very little guidance that has come out from the federal government for providers on the difference between a medical decision and a decision that is based purely on discrimination.[30] Many clinicians incorrectly presume that they have discretion to turn away patients with disabilities for reasons having nothing to do with the likely efficacy of the treatment itself.
We feel that clarifying that Section 1557 of the Affordable Care Act prohibit discrimination on the basis of disability in health care treatment options as well as “health care programs” would support the anti-discriminatory purpose of the revisions.
(ii) Prescription Drugs
Health plan enrollees living with chronic health conditions and other disabilities have witnessed discriminatory benefit design by some insurers, particularly in the coverage of prescription medications, which many beneficiaries living with chronic and serious health conditions rely on to remain healthy and alive. Some marketplace plans are placing all or almost all medications to treat a certain condition on the highest cost tier.
In the preamble of the Notice of Benefit and Payment Parameters for 2016 and in the 2016 Letter to Issuers, HHS has gone on record and stated that these practices could be discriminatory. In the Letter to Issuers, CMS cautions issuers from discouraging enrollment of individuals with chronic health needs and provided examples of discriminatory plan designs. One example identified was “if an issuer places most or all drugs that treat a specific condition on the highest cost tiers, that plan design might effectively discriminate against, or discourages enrollment by, individuals who have those chronic conditions.”
In order to protect beneficiaries and to provide clarity to state and federal regulators, DREDF urges HHS to include in regulatory language the practice of placing all or nearly all medications to treat a certain condition on the highest tier to be discriminatory.
In addition, plan enrollees with disabilities have experienced other design benefits that amount to
discrimination, including not covering certain medications or not following treatment guidelines, imposing excessive medication management tools such as unreasonable prior authorizations and/or step therapy, charging patients high cost sharing, requiring patients to “try” lower tier drugs before accessing a higher tier, and having narrow provider networks.
Therefore, in the final rule or through further guidance or FAQs, DREDF recommends that HHS stipulate that employing these types of practices is clearly defined as discrimination. Standards and parameters for benefit and plan design should be detailed in the final rule, along with acceptable practices. Unfortunately, the proposed rule is completely silent in this area and regulators, beneficiaries, and insurers are not provided with any clarity on what constitutes discrimination.
(iii) Habilitative and Rehabilitative Services and Devices
EHB benchmark plans and qualified health plans (QHPs) often demonstrate discriminatory benefit design in providing coverage for habilitative and rehabilitative services and devices. Within this category, people with disabilities experience discrimination on the basis of age, disability, and the type or severity of their disability. Below are several examples of discrimination that OCR should include as examples of discrimination in its final rule on non-discrimination.
(a) Habilitation and Developmental Disability:
Habilitation refers to services or devices that help people gainor maintain skills or functioning that they have never had. Rehabilitation refers to services or devices that help people re-gain or maintain skills or functioning that they have lost due to illness or injury. People with developmental disabilities are routinely denied coverage for habilitative services, such as physical therapy, needed to gain skills or improve functioning while an identical service is provided to individuals who would require rehabilitative care to restore functioning. We contend that these types of blanket service exclusions should be considered “unlawful on its face” in the same manner that is proposed to apply to gender transition-related care, as excluding habilitation coverage systematically denies services for people with developmental disabilities and is prohibited discrimination on the basis of disability.
Essential Health Benefits are required to cover habilitation. However, a few insurers have limited the availability of habilitative services and devices to people with specific diagnoses or developmental disabilities, at the exclusion of people with similar disabilities, functional limitations, or health care needs. The essential health benefit category of rehabilitative and habilitative services and devices is a broad grouping of services and supports that benefit a wide variety of people with disabilities, and remediate a wide variety of developmental conditions. The Congressional intent of this provision was expressed by The Honorable George Miller, Chairman of the House Committee on Education and Labor, a committee with primary jurisdiction over the House health reform bill, when he explained that the term rehabilitative and habilitative services:
“…includes items and services used to restore functional capacity, minimize limitations on physical and cognitive functions, and maintain or prevent deterioration of functioning. Such services also include training of individuals with mental and physical disabilities to enhance functional development.” [Congressional Record, H1882 (March 21, 2010)].
Limiting the coverage of habilitative services and devices to people with certain disabilities is discriminatory towards people with other disabilities and fails to ensure that coverage decisions focus on the individualized health care needs of each person.
The opposite situation also occurs, where the particular devices needed by people with specific types of
disabilities are excluded from coverage, seemingly without any actuarial evidence whatsoever. California’s benchmark plan, which is the Kaiser small business plan, has always contained a $2000 annual cap on DME. More recently, Kaiser has issued metal plans in Covered California that arbitrarily split Durable Medical Equipment (DME) in to two categories: “DME” and “Supplemental DME.” Wheelchairs are apparently only covered in the Supplemental DME category. In most plans supplemental DME is not covered at all, while in others, supplemental DME is covered with a $2000 annual cost cap. The fact that wheelchairs are medically necessary as well as critical to the functional capacity of some individuals with disabilities to live in the community seems to be irrelevant. There has never been any disclosure of actuarial evidence behind imposing categorical exclusions and unique coverage limits on a targeted rehabiliation/habilitation device such as “wheelchairs. There is only a historical practice of discrimination that insurance companies continue because no one stops them from doing so. This practice wreaks havoc with a number of broad principles established under the ACA relating to no discrimination for pre-existing conditions, establishing Rehabilitation/Habilitation services and devices as an Essential Health Benefit category, and the prohibition of special annual and lifetime coverage limits.
(b) Hearing Aids:
In the most recent release of benchmark plans for determining Essential Health Benefits for the 2017 plan
year, the Habilitation Benefits Coalition found the following limits in on coverage for hearing aids in all 50 states and the District of Columbia.
- The benchmark plan offers no coverage for hearing aids in Alabama, Alaska, Arkansas, California, Florida, Georgia, Idaho, Indiana, Iowa, Kansas, Michigan, Mississippi, Montana, Nebraska, North Dakota, Ohio, Pennsylvania, South Carolina, South Dakota, Utah, Vermont, Virginia, Washington State, Washington, DC, West Virginia, Wyoming.
- The benchmark plan covers hearing aids only for children, while denying coverage for adults in Colorado, Connecticut, Delaware, Illinois, Kentucky, Louisiana, Massachusetts, Maryland, Maine, Minnesota, Missouri, New Jersey, New Mexico, North Carolina, Oklahoma, Oregon, Rhode Island, Tennessee, Texas, Wisconsin.
Hearing aids and similar technologies are “rehabilitative or habilitative devices” and, as such, must be covered under every state’s EHB benefit package for 2017. Failure to cover hearing aids and similar technologies violates both the ACA’s statute and regulations. Failing to cover hearing aids discriminates against people with hearing impairment, and coverage of hearing aids for children only and not for adults also violates the ACA prohibition against discrimination in plan designbased on age.
(c) Prosthetics and Orthotics:
The 2017 Essential Health Benefits benchmark plan for New York State initially included a policy limiting coverage to only one external prosthetic device, per limb, per lifetime. This would have served as the baseline for QHPs in the New York State Health Insurance Marketplace and had disastrous implications for people with disabilities who need prosthetics. The policy would have effectively meant zero coverage for the individual based on their disability once the useable life of their first prosthetic had ended. Limiting the number or frequency of replacements for prosthetics or orthotics also has a discriminatory impact on children with disabilities, who need frequent replacements as they grow. Such policies not only violate the ACA requirements for coverage of habilitative and rehabilitative services and devices, but also provides an example of the kind of limits and utilization management that specifically target people with disabilities, and are discriminatory.
(d) Visit Limits:
The ACA, in describing requirements of Essential Health Benefit packages, requires that the Secretary “not make coverage decisions…or design benefits in ways that discriminate against individuals because of their age, disability, or expected length of life.” (ACA Section 1302(b)(4)(B)). Section 1557 further prohibits discrimination on the basis of disability. Finally, the ACA disallows monetary caps on coverage. However, EHB benchmark packages approved by the Secretary continue to include hard limits on the coverage of habilitative and rehabilitative services and devices. Hard limits on a total number of visits allowed to particular providers are a de-facto annual monetary cap on coverage, which violates the ACA. Further, these limits discriminate against people with more significant disabilities who need higher levels of therapy, thus violating Sections 1302 and 1557. Limitations on the number of covered visits without regard for medical necessity, best medical practices, or the extent of therapy prescribed to the individual discriminates against people with more significant disabilities who need this extensive habilitation or rehabilitation in order to gain, regain, or maintain functioning.
In the proposed regulatory language, Section 92.207(b)(1) prohibits a covered entity from limiting a health insurance plan, policy or other health coverage, or limiting coverage of a claim, or imposing limitations on the basis of an enrollee’s disability. Section 92.207(b)(2) prohibits a covered entity from employing marketing practices or benefit designs that discriminate on the basis of disability. Any caps on coverage of habilitative or rehabilitative services or devices would violate these proposed regulations. OCR should finalize these regulations and then issue guidance describing this discrimination.
Subpart D — Enforcement
Individual Enforcement:
We urge the Department to clarify that disability discrimination claims brought under Section 1557 claims may be privately enforced and that damages are available. The preamble correctly notes that “based on the statutory language [that enforcement mechanisms under Title VI, Title IX, the Age Act, or Section 504 apply for violations of Section 1557], a private right of action and damages for violations of Section 1557 are available to the same extent that such enforcement mechanisms are provided for and available under Title VI, Title IX, Section 504, or the Age Act with respect to recipients of Federal financial assistance.”[31] It is well established that claims under Section 504 may be privately enforced and that damages are available. The same is true of the other listed statutes. To provide clarity, however, it is critical that this language be included in the text of the final rule and not simply in the preamble.
Government Enforcement:
An individual, complaint-driven system of enforcement is particularly limiting in healthcare for a number of reasons. First, many individuals are understandably reluctant to submit individual complaints. For example, the need for ongoing relationships with healthcare providers (and particularly specialists in practice areas where there is a shortage of practitioners, and in rural areas where practitioners are in short supply) makes it difficult for individuals to file complaints concerning discrimination by providers. Second, individual complaints cannot typically produce resolutions in time to address pressing health care needs. Third, the complexity of ACA implementation may make it difficult for many forms of discrimination to be addressed through the individual complaint process. Fourth, individual complaints are often a poor vehicle for creating needed systemic change. OCR should prioritize enforcement of Section 1557 with respect to systemic problems and should involve the Justice Department (DOJ) whenever DOJ has concurrent authority, including referring matters to DOJ for litigation whenever appropriate.
In addition, we urge that OCR, as part of its efforts to enforce Section 1557, work with CMS to ensure that CMS contracts with state health care agencies and MCOs include non-discrimination provisions and consequences for failing to comply with these provisions. OCR should also ensure that compliance reviews concerning accessibility do not rely on self-evaluations and also include unannounced visits to providers and health care entities to review accessibility.
Intersectional Bases of Discrimination
While disability affects people of all races, ethnicities, genders, languages, sexual orientations, and gender identities, this does not mean that impairment occurs uniformly among racial and ethnic groups. Disability is identified in differing ways among surveys, but national sources indicate that disability prevalence is highest among African Americans, who report disability at 20.5 percent compared to 19.7 percent for non-Hispanic whites, 13.1 percent for Hispanics/Latinos and 12.4 percent of Asian Americans.[32] Disability prevalence among American Indians and Alaskan Natives is 16.3 percent.[33] In raw numbers, over 10.8 million non-institutionalized people with disabilities aged 5 and over are estimated to be members of ethnic minorities.[34] An Institute of Medicine report has already observed that there are “clear racial differences in medical service utilization rates of PWD that were not explained by socioeconomic variables,” and “‘persistent effects of race/ethnicity [in medical service utilization] could be the result of culture, class, and/or
discrimination.'”[35] People with disabilities are likely to fall into more than one protected group, and the relationship between race and disability has cumulative impact on creating health disparities. Nondiscrimination protections must take into account these intersectional elements of living with disability. For example:
- Diabetes often leads to vision loss, but most modern glucometers have a flat screen interface that is inaccessible to blind people. Adults with disabilities have a 400 percent elevated risk of developing
Type II diabetes.[36] Diabetes is also a rapidly growing health challenge among Asian Americans and Pacific Islanders who have immigrated to the United States, affecting about 10 percent of Asian Americans, with 90-95 percent of these having type 2 diabetes.[37] - 4.6 percent of Deaf people are infected with HIV/AIDS, four times the rate for the African-American population,[38] the most at-risk racial group in the U.S.[39] Measures to target HIV/AIDS outreach and information to LGBT people of color who experience multiple health barriers must also consider the factor of hearing impairments on effective communication of health information.
- Three out of five people with serious mental illness die 25 years earlier than other individuals, from preventable, co-occurring chronic diseases.[40] At the same time, African Americans with severe mental health disabilities are less likely than whites to access mental health services, more likely to drop out of treatment, more likely to receive poor-quality care, and more likely to be dissatisfied
with care.[41] Asian Americans and Hispanics are less than half as likely as whites to receive mental health treatment.[42] People with mental health disabilities are at greater risk of developing chronic conditions, a disparity compounded among people wit mental health disabilities from racial and ethnic minorities. - People with significant vision loss experience a greater prevalence of obesity, hypertension and heart disease, and cigarette use than the general public.[43] People who are Hispanic have higher rates of visual impairments than people who are African American, and both groups have higher rates of vision impairment than people who are white.[44]
- 15 percent of PWD report not seeing a doctor due to cost, compared to 6 percent of the general population.[45] Adults with annual household incomes of less than $25,000 are more likely to report having a disability than adults with an annual household income equal to or greater than $25,000.[46] People with disabilities and members of racial minorities often share socio-economic characteristics and related health access barriers due to the expense of maintaining health with a disability. Anti-discrimination efforts related to cost-sharing should account for this intersection of poverty, disability, and racial minority status.
- Among people who are deaf, women of color appear to experience the greatest health disparities and difficulty accessing appropriate health care. They tend to have lower incomes and poorer health, and to be less educated compared with white women. Among women of color, African American Deaf women appear to experience the greatest health disadvantages.[47]
We have two recommendations relating to the needs of people with disabilities who also intersect with other personal characteristics that are protected under Section 1557.
- The regulations need to clarify that covered entities, when addressing the communication needs of a Deaf individual or another race or ethnicity, must address the unique accommodation needs of that individual. The provision of print notes in another language, or of American sign-language, can be ineffective for complex medical communications whether provider individually or in concert.
- Data collection on disability status, in sufficient granularity to enable covered entities to discern and develop the provision of appropriate accommodations, needs to be addressed with the regulation. Considerable strides have been made within a number of state marketplaces and in the federal marketplace toward the voluntary gathering of important information on race and ethnicity. This has not extended to disability status. Section 4302 of the ACA concerning the need for survey information concerning how and where the health needs of people with disabilities are met must be sufficiently supported and mandated before the needs of individuals who are “at the intersection” can be addressed.
Thank you again for the opportunity to comment on the proposed 1557 rule. Please do not hesitate to contact us if there are any questions about the above.
Yours Truly,
Silvia Yee
Senior Staff Attorney
[1] See 80 Fed. Reg. at 54174 and 54195.
[2] Civil Rights Issues in Health Care Delivery, A Consultation Sponsored by the United States Commission on Civil Rights, Washington, D.C., April 15-16,1980 at 855.
[3] Id. at 856-7, citing 110 Cong. Rec. 13378 (1964).
[4] Id. at 857, citing 110 Cong. Rec. 13345,
13346 (1964).
[5] Hearing before Subcommittee No. 5 of the House Committee on the Judiciary, 88th Cong. 1st Sess. 1545-1546 (1963).
[6] Id. at 854.
[7] Id. at 863.
[8] See Medicare Enrollment Application, Physicians and
Non-Physician Practitioners, CMS-8551.
[9] 80 Fed. Reg. at 54,174, see also 45 C.F.R. § 86.2(g)(1)(ii).
[10] 80 Fed. Reg. at 54,174.
[11] Id. at 854.
[12] See 42 C.F.R. Sec 405.900 et seq Please note that even non-participating physicians not billing on an assigned basis can be parties to an appeal. 42 C.F.R. Sec.405.908 (b)(4).
[13] See Medicare Learning Network, Medicare Parts A
& B Appeals, ICN 006562 (Feb. 2015).
[14] An article in Health Affairs noted:
David Barton Smith, Racial and Ethnic Health Disparities and The Unfinished Civil Rights Agenda, 24 Health Affairs 317 (2005) (citations omitted).
[15] Civil Rights Issues, supra note 25, at 863.
[16] See Zulman D.M. et al. (2011) Examining the Evidence: A Systematic Review of the Inclusion and Analysis of Older Adults in Randomized Controlled Trials, Journal of General Internal Medicine, 26(7), 783-790; Chronic Disease Prevention and Control Research Center at Baylor College of Medicine. Major Deficiencies in the Design and Funding of Clinical Trials: A Report to the Nation Improving on How Human Studies Are Conducted (April 2008).
[17] Developing Quality of Care Measures for People with Disabilities: Summary of Expert Meeting. AHRQ Publication No. 10-0103, September 2010. Rockville, MD: Agency for Healthcare Research and Quality, available onlineat: http://www.ahrq.gov/populations/devqmdis/ (“In recent years, the National Institutes of Health (NIH) and AHRQ have required investigators submitting grant applications to explicitly address the inclusion of persons by sex and race and ethnicity. Both NIH and AHRQ grant applicants must justify the exclusion of people by sex, race, and ethnicity. NIH applicants must also address the inclusion of children and justify their exclusion. Beyond women and racial and ethnic minorities, AHRQ requires grant applicants to consider including the following “priority populations”:inner-city residents; rural residents; low income persons; children; elderlypeople; and those with special health care needs, including individuals withdisabilities and those who need chronic care or end-of-life health care.”)
[18] 80 FR 54181.
[19] Available at:
http://citeseerx.ist.psu.edu/viewdoc/download?rep=rep1&type=pdf&doi=10.1.1.204.2449 [last visited October 14, 2015].
[20] Section 6 of the UFAS is a relatively short section
on “Health Care” that requires an entrance canopy or overhang over health care facility or building entrances to protect from weather, and otherwise deals exclusively with patient bedroom measurements in such facilities.
[21] Available at: http://www.cfm.va.gov/til/accessibility.asp. [last visited October 14, 2015].
[22] Mudrick NM, Breslin ML, Liang M, and Yee S. “Physical Accessibility in Primary Health Care Settings: Results from California On—Site Reviews.” Disability
and Health Journal 5 (2012) 159-167; Lagu, T et al. “Access to Subspecialty Care for Patients with Mobility Disabilities: A Survey.” Ann. Intern. Med. (2013) 158: 441-446.
[23] See “CMS Equity Plan for Improving Quality in Medicare.” Centers for Medicare and Medicaid Services, Office of Minority Health. September 2015.
Accessed October 16, 2015. http://www.cms.gov/About-CMS/Agency-Information/OMH/OMH_Dwnld-CMS_EquityPlanforMedicare_090615.pdf; Krahn, Gloria L., Deborah Klein Walker, and Rosaly Correa-De-Araujo. “Persons With Disabilities as an Unrecognized Health Disparity Population.” American Journal of Public Health. Vol 105, No. S2
(2015): S198-206.
[24] Department of Health and Human Services, Centers for Medicare & Medicaid Services, Guidance to States using 1115 Demonstrations or 1915(b) Waivers for Managed Long Term Services and Supports Programs 3 (May 20, 2013) (“All MLTSS programs must be implemented consistent with the Americans with Disabilities Act (ADA) and the Supreme Court’s Olmstead v. L.C. decision. Under the law, MLTSS must be delivered in the most integrated fashion, in the most integrated setting, and in a way that offers the greatest opportunities for active community and workforce participation.”). See also Id. at 10 (“In keeping with the intent of the ADA and Olmstead decision, payment structures must encourage the delivery of community-based care and not provide disincentives, intended or not, for the provision of services in home and community-based settings”), and 13 (“States that exclude specific services from their MLTSS programs will be expected to routinely assess whether there is any negative impact as a result of the exclusion and whether there are any violations of federal requirements, including the ADA or Olmstead”).
[25] Non-discrimination laws such as the ADA reach
discrimination among different disability groups. See Olmstead v. L.C., 527 U.S. 581, 602 n. 10 (1999).
[26] Disability Rights Education & Defense Fund,
Comments, Re: Docket No. HHS-OCR-2013-0007 (Request for Information Regarding Nondiscrimination in Certain Health Programs or Activities) (2014), available at https://dredf.org/wp-content/uploads/2013/10/1557-Disability-Comment-Final.pdf.
[27] Levenson JL, Olbrisch ME. “Psychosocial evaluation
of organ transplant candidates: A comparative survey of process, criteria, and outcomes in heart, liver, and kidney transplantation.” Psychosomatics 1993 Jul-Aug;34(4):314-23.
[28] Richards CT, Crawley La Vera M, Magnus D. “Use of
neurodevelopmental delay in pediatric solid organ transplant listing decisions: Inconsistencies in standards across major pediatric transplant centers.” Pediatric Transplantation 2009:13:843—850.
[29] ASAN Organ Transplantation Policy Brief, http://autisticadvocacy.org/wp-content/uploads/2013/03/ASAN-Organ-Transplantation-Policy-Brief_3.18.13.pdf.
[30] ASAN Organ Transplantation Policy Brief.
[31] 80 Fed. Reg. 54192 (Sept. 5, 2015).
[32] Brault, Matthew, Americans With Disabilities: 2005,
Current Population Reports, P70¬117, U.S. Census Bureau, Washington, DC, 2008. Many of the differences between the disability rates by race and Hispanic origin can be attributed to differences in the age distributions of their populations. For example, Hispanics are predominantly younger than non-Hispanic
whites.
[33] U.S. Census Bureau, 2009 American Community Survey,
S1810. Disability Characteristics 1 year estimates, available at
http://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=bkmk
[34] Id. The 10.8 million figure is derived from
subtracting the total number of PWD who identify as non-Hispanic or Latino white from the total number of those with a disability aged 5 and over.
[35] Institute of Medicine (IOM). 2007. The Future of
Disability in America. Washington, DC: The National Academies Press, p. 92.
[36] Seth Curtis and Dennis Heaphy, Disability Policy
Consortium: Disabilities and Disparities: Executive Summary (March 2009), p. 3.
[37] Asian American Diabetes Initiative, Joslin Diabetes
Center (2010), http://aadi.joslin.org/diabetes-in-asian-americans
[38] Curtis & Heaphy, p. 8.
[39] AVERT,HIV and AIDS in the United States of America (USA), http://www.avert.org/professionals/hiv-around-world/western-central-europe-north-america/usa#footnoteref10_yr5z19g
[40] Assoc. of University Centers on Disabilities,
“Letter to Kathleen Sebelius”
https://www.aucd.org/docs/policy/health_care/CLAS_StandardsDisabilityLetter%201-2011.pdf
Citing (Colton & Manderscheid, 2006; Manderscheid, Druss, & Freeman, 2007.
[41] Whitley, R., & Lawson, W.. (2010). The Psychiatric Rehabilitation of African Americans With Severe Mental Illness. Psychiatric Services, 61(5), 508-11.
[42] 2008 National Healthcare Disparities Report. Table
15_3_1.1a & 15_3_1.1b http://www.ahrq.gov/qual/qrdr08/index.html
[43] Michele Capella-McDonnall, “The Need for Health
Promotion for Adults Who Are Visually Impaired,” Journal of Visual Impairment and Blindness 101, no. 3 (March 2007).
[44] Id. Note that a vision impairment is a visual
disability not correctable by glasses or other modifications.
[45] Curtis & Heaphy, p. 3.
[46] Curtis & Heaphy, p. 3.
[47] National Council on Disability, 2009.