February 14, 2012
Submitted electronically to: EssentialHealthBenefits@cms.hhs.gov
The Honorable Kathleen Sebelius
Secretary of Health and Human Services
U.S. Department of Health and Human Services
200 Independence Avenue, SW
Washington, DC 20201
RE: Essential Health Benefits Bulletin
Dear Secretary Sebelius:
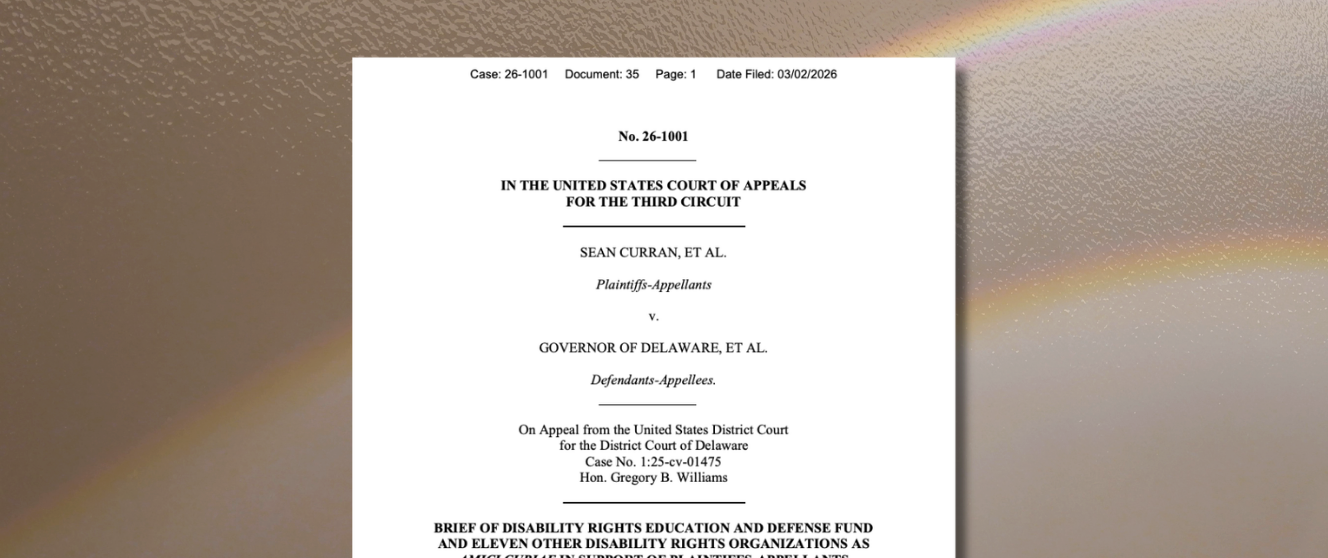
Thank you for the opportunity to comment on the Essential Health Benefits (EHB) Bulletin released December 16, 2011 by the Center for Consumer Information and Insurance Oversight. The Disability Rights Education and Defense Fund (DREDF) is a leading national law and policy center that advances the civil and human rights of people with disabilities through legal advocacy, training, education, and public policy and legislative development. We are a cross-disability organization, and submit these comments because the unavailability of insurance and underinsurance are long- standing and fundamental concerns of people with disabilities. The enactment of the Affordable Care Act (ACA), and particularly its non-discrimination provisions concerning pre-existing conditions, annual and lifetime benefit limits, and disability discrimination in general, will enable people with disabilities to come closer to achieving health insurance services and coverage that are fundamental to maintaining health, function, employment, civic and social engagement, and residence in the community. When we speak of people with disabilities in the context of health insurance, we emphasize that we represent not only the interests of people who currently have chronic diseases and disabilities, but also millions of individuals of all ages who will acquire functional impairments in the future, and who think that they have health insurance that will give them access to the treatments, therapies, and devices that they need to go on with their lives.
DREDF has contributed and signed on to EHB letters submitted, or to be submitted, by the Leadership Conference on Civil Rights (LCCR), the Consortium for Citizens with Disabilities (CCD), and the Independence Through Enhancement of Medicare and Medicaid (ITEM) Coalition, and supports the excellent points raised by both the National Health Law Project (NHeLP), and Access Living and the Coalition for Disability Health Equity in their letters. We do not intend to repeat the comments made in those letters. Instead, we would like to focus closely on an ongoing trend in small group life insurance in California that illustrates the great risk to people with disabilities of allowing states “to select a single benchmark to serve as the standard for qualified health plans” in the state’s exchange, and for plans in that state’s individual and small group markets. As discussed in the Bulletin, the benchmark approach would serve to entrench discrimination that is already imbedded within plan benefit design if it is not explicitly subject to clear federal standards for each benefit category that abolish discriminatory benefit limits and scopes of coverage.
Benchmark Approach and Entrenching Discrimination in Benefit Design
California’s Health Benefit Exchange Board recently submitted joint comments with the State’s Managed Risk Medical Risk Insurance Board and the Departments of Health Care Services, Managed Health Care, and Insurance.[1]At p. 4 of the January 30, 2012 letter, the authors interpret as follows the Bulletin’s statement at p. 8 that “[t]he selected benchmark plan would serve as a reference plan, reflecting both the scope of services and any limits offered by a ‘typical employer plan’ in that State as required by section 1302(b)(2)(A) of the Affordable Care Act.” [emphasis added]
1) We would interpret the language in the Bulletin regarding benefit scope and limits to mean that once a state selects a specific benchmark, all of the elements of the “scope of services” and “limits” in the selected policy or contract – benefit definitions, coverage limitations or service caps, coverage exclusions, key terms affecting coverage (e.g., medical necessity, experimental), service utilization controls (e.g., prior authorizations, site or setting) – would be incorporated into the state definition of essential health benefits. If this interpretation is not accurate, please clarify.
2) Health coverage products, particularly small employer coverage, often feature a set of baseline benefits along with optional coverage riders that either add covered services or modify limitations for existing covered services. The Bulletin language implies that, by selecting the plans with the largest enrollment, the most popular optional riders accompanying a specific benchmark product would be included as essential health benefits. If this interpretation is not accurate, please clarify.
Both the ACA and the Bulletin distinguish between the benefits that a plan must cover, and the cost sharing features, such as deductibles, copayments, and coinsurance, attached to those benefits. From the viewpoint of the individual consumer, however, the question of whether a plan will truly meet their needs hinges on the critical factor of scope and coverage limits as much as the bare fact of coverage. Future guidance by the Department of Health and Human Services (HHS) will cover plan cost sharing and the calculation of actuarial values, as indicated in the opening paragraph of the Bulletin, but if existing scope and coverage limitations can be wholly imported into the benefit package when states adopt their benchmark plans, the value of insurance coverage to consumers will be severely reduced. A minimum co-pay or deductible on a benefit that will still cover only a fraction of the actual cost of a necessary benefit can only be described as “gold” or “platinum” in the most euphemistic sense. Furthermore, the benchmark approach described in the Bulletin will deeply undercut the ACA’s non- discrimination provisions.
First, Section 1302(b)(4)(D) of the Act requires the Secretary to ensure “that health benefits established as essential not be subject to denial to individuals against their wishes on the basis of the individuals’ age or expected length of life or of the individuals’ present or predicted disability, degree of medical dependency, or quality of life.” Individuals with functional impairments and/or chronic conditions may not be explicitly excluded from a plan on the basis of diagnosis or condition, but if a plan is allowed to simply preserve arbitrary coverage limitations on the therapies and devices that such individuals need to maintain life and health in the community, then that health benefit has effectively been denied, irrespective of whether Congress intended its inclusion within the EHB list.[2]
Second, sections 1302(b)(4)(B) states that the Secretary cannot make “coverage decisions, determine reimbursement rates, establish incentive programs, or design benefits in ways that discriminate against individuals because of their age, disability, or expected length of life.” The decision to abdicate responsibility for actively specifying EHB standards by leaving coverage, reimbursement, incentive and benefit design to states and plans in the name of “flexibility” remains a decision made by the Secretary that results in discrimination against individuals. Similarly, Section 1302(b)(4)(C) places the Secretary under a proactive obligation to “take into account the health care needs of diverse segments of the population, including women, children, persons with disabilities, and other groups.” This purpose is not served for people with disabilities and other groups enduring health and healthcare disparities unless the Secretary (1) clearly and unambiguously ensures that states and plans meet the requirements of a specified non- discriminatory EHB minimum benefit floor across all ten categories, and (2) establishes mechanisms for encouraging and incentivizing state and plan innovation to both maintain existing mandates that go beyond the minimum floor, and develop additional innovative products that will offer benefits “in excess” of EHB, as expressly provided for in Section 1302(b)(5) of the ACA. DREDF appreciates the “transition period” mentioned in the Bulletin that would enable states to defray the costs of additional state mandated benefits that go beyond the EHB by choosing a benchmark that is subject to state mandates. However, this incentive is insufficient to counter the enormous pressure on states to both attempt the repeal of existing mandates, and to resist passing any future mandates, including mandates clearly needed to redress short-sighted health policy decisions and private insurance limitations that were initially imposed on the basis of extremely limited or no evidence.
Third, the probation in section 1001(1) on lifetime or annual benefit limits on the dollar value of benefits offered in group and individual health insurance coverage after January 1, 2014 is simply rendered illusory if such limits can continue as integrated components of a state’s EHB benchmark. While the “grandfathering” of pre-2014 plans with lifetime or annual benefit limits on EHB enables such plans to continue existing in a state’s marketplace, it was clear that such products would eventually face extinction as plans were adopted and upgraded to remain competitive. This is not necessarily the case if lifetime and annual benefit limits, and other coverage limitations are imbedded in the EHB. The Bulletin gives no concrete plan for how HHS will discharge its obligation to periodically assess EHB. The general admonition that health insurance issuers “would be expected on an ongoing basis to reflect improvements in the quality and practice of medicine” does very little to offset or eliminate coverage limitations that were not imposed on the basis of medical evidence or review in the first place, and existing limitations presumably could remain undisturbed and not reviewed for many years..
What follows is one concrete example of an imbedded discriminatory practice common in California’s small group insurance products. While this specific example focuses on Durable Medical Equipment (DME), it illustrates how private insurers make economically unwarranted and humanly unsustainable decisions about coverage and actuarial value. This one example is undoubtedly replicated across all ten EHB categories, within dozens of plan products, and among all fifty states. The benchmark approach may facilitate some degree of comparability among the insurance products offered in a single state, but it will do very little to remediate historic insurance discrimination against people with disabilities, bring health coverage to a baseline value between states, or alleviate the difficulties that adverse selection places on individuals with disabilities who cannot secure sufficient, affordable private coverage needed for working and living in the community.
Coverage of DME in California under Private Insurance
Durable Medical Equipment (DME) encompasses a variety of devices intended for ongoing use such as ventilators, crutches, wheelchairs, patient lifts, hospital beds, shower chairs, infusion pumps, and blood glucose monitors that help with such basic functions as breathing, mobility, using the restroom, and monitoring one’s health. Typically DME would be encompassed within the 10 EHB benefit categories identified in the ACA as “rehabilitative and habilitative services and devices,” as these are devices that are used to create, restore, improve, or maintain skills and function.[3]In the public context, insurance programs such as Medi-Cal[4] and Medicare cover DME when it enables people with an illness, injury, or impairment to maintain their health, get around in their homes, and contribute to their communities.[5]DME is critical to the health of people who use this equipment, and accounted for only .47% of total Medi-Cal costs in 2001.[6] California’s combined public, private, and out-of-pocket expenditures on DME are growing only half as quickly as the state’s overall healthcare expenditures.[7]
In recent years, up to 90% of California’s private small group health insurance plans placed an annual $2000 benefit limit on DME that could not be carried forward from one year to the next. Individual health insurance plans often imposed an annual DME benefit cap in addition to hefty monthly premiums and high deductibles. Almost half of California’s three million people with disabilities have private health insurance.[8]Within this privately insured group, a much smaller percentage of people rely on DME and are therefore directly affected by special caps and limitations on DME coverage. One estimate is that 2.3% of working-age Californians (18-64) with private insurance as their primary form of health coverage, roughly 326,000, need some form of DME.[9]DREDF became involved with the issue in 2007 after noting the trend and its deleterious impact on many colleagues and friends in the disability community who, despite being insured, were suddenly confronted with the need to pay out-of-pocket for such significant items as electric wheelchairs, which can cost $15,000 or more. The necessity for custom seating and additional musculoskeletal aids is not even included in this estimate.
DREDF and Disability Rights California (DRC) sponsored AB 754, a 2009-2010 bill that would have required private health insurers to cover DME in group and individual plans, and prevented plans from placing special coverage limitations on DME. Since the bill proposed a new health insurance benefit mandate, it had to undergo an independent analysis by the California Health Benefits Review Program (CHBRP) of its medical, financial, and public health impacts. The following highlights about DME users, coverage limitations, and the cost, usage, and health impacts of the proposed mandate are drawn from the June 24, 2010 CHBRP report to the 2009-2010 California State Legislature.[10]
- Many people with relatively high DME costs include persons in the following categories: (1) persons with conditions related to physical disabilities, such as musculoskeletal disorders; (2) persons with sequelae from traumatic injuries such as spinal cord injuries and head trauma; (3) respiratory diseases and related conditions requiring the use of home oxygen equipment; and (4) persons with diagnoses related to complications of the digestive system requiring DME for nutrition.
- Approximately 19,487,000 enrollees in DMHC-regulated plans and CDI- regulated polices have health insurance that would be subject to AB 754 (Table 1). The mandate would place requirements on plans and policies in both the group and individual markets. CHBRP surveyed the seven largest major health plans and insurers in California regarding DME coverage and the scope of provided DME benefits. Responses represented 82.37% of enrollees in CDI- regulated policies and 92.03% of enrollees in DMHC-regulated plans.[11]Combined, responses to this survey represented 90.45% of enrollees with privately funded health insurance.
- 18,185,538 (93.32%) enrollees have some coverage for DME. However, 10,294,137 (52.83%) enrollees have coverage for DME not currently in compliance with AB 754 because they face higher coinsurance or copayments for DME and services than for other medical benefits, or because they face annual DME benefit limits, or both. At the time of the study, 49% of enrollees in DMHC regulated private individual plans had non-compliant coverage, 74% had non-compliant coverage in the small group plans, and 61% had non-compliant coverage in the large group plans. Among CDI regulated private plans, 97% had non-compliant coverage in the individual market, 99% had non-compliant coverage in the small group market, and 100% had non-compliant coverage in the large group market.
- For non-compliant plans and policies, typical average cost-sharing levels for DME ranged by market segment from 21% to 30%, compared with cost-sharing levels ranging from 0-29% for plans that offered DME cost-sharing parity. The average coinsurance rate was 13.61% among non-compliant plans. 6.68%, or approximately 1.3 million plan/policy enrollees had no DME coverage at all.
- 33.16% of enrollees with DME coverage were subject to an average annual benefit limit of $3,187. This sharply contrasts with annual benefit limitations applied to other health benefits as the large majority of plans and policies either have no annual limit or have very high annual limits that affected a very small number of insured persons (e.g., .6% of enrollees in the group market and 0.1% of enrollees in the individual market. Such limits averaged $70,000 for group policies and $100,000 for individual purchased policies.
- CHBRP estimated the cost impact of the mandate to be $135,933,000 (or 0.18%) in total health care costs in California (Table 1). Across all markets, including those that are unaffected by AB 754 because they already cover DME at parity,[12]premiums were expected to increase by $276,306,000 or 0.39% (Table 6). In dollar terms, the increases ranged from 0.022% or $0.50 per member per month (PMPM) to 0.241% or $1.13 PMPM in CDI-regulated policies, and from 0.099% or $1.01 PMPM to 0.846% of $5.13 PMPM in DMHC-regulated plans.[13]
- There are an estimated 55 DME users per 1000 plan/policy enrollees per year who spend an estimated average annual cost of $743.56 on DME. 2.73% of DME users in currently non-compliant plans have annual DME expenses in excess of their annual DME benefit limit. CHBRP estimated that AB 754 would increase of $52.01 (6.99%) per DME user per year due to increase DME utilization and related expenses. However, there would be a substantial reduction in administrative and financial burden for 72,000 newly covered DME users as well as for the 556,000 DME users with an increase in their scope of DME coverage.
- Overall, CHBRP expected minimal impacts on access to and availability of DME and services as a result of AB 754. To the extent that cost sharing would be reduced and limits removed, access would be expected to increase for the small number of enrollees who seek equipment in excess of the annual benefit limit. Nonetheless, utilization review and medical management were not affected by the Bill and were expected to mediate the response of the health plans and policies to this increase in demand.
- There is insufficient evidence to assess the impact of health insurance coverage for DME on use of DME and health outcomes for persons who use DME. The few studies that have been conducted suggest that need is the primary factor associated with use of DME. No studies were found that specifically address the effects of increasing annual or lifetime limits for DME coverage on DME usage or the impact of reducing deductibles, coinsurance, or copayments for DME on such usage. No studies were found that address the impact of coverage for DME on health outcomes.
DME coverage in California and the CHBRP study illustrate how private plans and insurance companies make benefit coverage decisions that can have profoundly negative financial and health consequences on those impacted. DME coverage limitations mean that people with disabilities will delay acquiring needed DME items, or eventually assume the high out-of-pocket cost but give up needed medications, food, or even job opportunities or life in the community. There is no need for insurance companies or plans to outright refuse to cover people without disabilities, which would directly run into the non-discrimination prohibition of the Americans with Disabilities Act if the ACA is interpreted to allow benefit design that inevitably leads to adverse selection. DME restrictions were initially made by only some companies and plans and then quickly swept through the entire industry,[14]with very little evidence of actuarial or policy analysis behind the decisions. There is also very little indication that the few cents or dollars PMPM “saved” by sacrificing the small number of enrollees who incur DME costs above annual DME benefit limits have actually been passed on to consumers. Premiums have risen throughout this time period and California consumers have certainly not been explicitly asked about their willingness to assume the risk of high DME cost shares, coinsurance, or annual benefit limits if they should, for example, be in a car accident or acquire a chronic condition and need DME. It could be argued that the low numbers of individuals directly impacted by DME coverage limitations somehow justifies the imposition of such limitations, but the low numbers also fuel the counter-argument that covering DME without coverage limitations provides minimal cost-savings overall.
Ultimately, cutting or limiting DME coverage for people with disabilities hardly makes a dent in overall private insurance costs, but deeply impacts people with disabilities who rely on various types of DME to maintain health and independence, and to live full lives, work, and raise their families in the community.
ACA Non-Discrimination Provisions in Enforceable EHB Guidance
The ACA non-discrimination provisions must be directly applied to and incorporated within enforceable federal EHB benefit design rules for the reasons set out above. The rules should explicitly state that insurance plans and policies must not discriminate on such grounds as disability, age, degree of medical dependency, expected length or quality of life,[15]race, color, national origin, sex, gender identity, or sexual orientation in their benefit design, neither within any given EHB category nor in the design of the overall EHB package. HHS’s clear national designation of the treatments, therapies, and devices that must minimally be included within each EHB category, and establishment of a federally monitored and incentivized procedure for adding to or updating benefit categories, will greatly alleviate deeply entrenched adverse selection practices, but not entirely alleviate the discriminatory design and delivery of EHB services.
The federal rules must also ensure the physical and programmatic accessibility of health plan and policy services to people with disabilities. Strong non-discrimination prohibitions in benefit design should bring the long-standing discriminatory exclusion of hearing aids from rehabilitation/habilitation coverage to an end, but the hearing impaired or Deaf individual’s need for effective communication must be addressed in the delivery of the benefit or the benefit will not be realized in practice. As another example, mental health and substance use disorder services is one of the 10 EHB categories, and may also be covered within a given state’s benchmark, but if coverage reimbursement rates fail to account for a deaf individual’s need for ASL or a visually impaired individual’s need for all written materials in an alternative format such as large print font or CD, that “essential benefit” will not be meaningful. The same is true for a woman using a wheelchair who has the right to preventive services such as a PAP smear and mammogram, but cannot find a provider with height adjustable exam tables or mammography imaging equipment and the willingness to spend the additional time that may be needed to affect a safe transfer. As stated above, it is not enough to rely on the statutory prohibition of discrimination without direction in the regulations. Health plans, in particular, must establish the capacity, and demonstrate willingness, to examine their benefit design practices, policies, and administrative procedures to remove historic discriminatory barriers that have long denied equally effective care to people with disabilities, including LEP individuals, minorities, and LGBT individuals who face multiple barriers to care.
Conclusion
There is little point to enacting a law that would prevent one form of insurance discrimination, such as a refusal to insure individuals with pre-existing conditions, while simultaneously allowing another form of discrimination, such as a refusal to cover the treatments, devices, and prescriptions that individuals with pre-existing conditions require to maintain health and function. If the ACA is truly intended to make actuarially valuable insurance and health care coverage readily available and affordable to people with disabilities, then it must establish minimum coverage requirements within and across the EHB categories, and ensure non-discrimination in benefit design. Non- discrimination provisions must also clearly extend to the operation of traditional gate- keeping mechanisms such as medical necessity and outdated rules for how treatments and devices must be obtained or used (e.g., Medicare “homebound” requirement for certain DME items). The ability to obtain insurance coverage and needed health services and devices cannot depend upon such arbitrary factors as whether a low- incidence condition has or has not been included in “gold standard” medical research, or whether a covered individual does or does not have employment or a social life.
Finally, the EHB rules must also address the need for plan transparency and beneficiary representation in decision-making and oversight bodies, strong non-exhaustive administrative complaint and appeal mechanisms, and robust federal and state monitoring and enforcement procedures, including the reporting and public availability of key disability-specific data measures. The viewpoint of people with disabilities is especially important, and must be represented in, any procedures for updating benefit packages. The need for the disability representation is illustrated by the second point of clarification raised by the State of California in its EHB comment letter, concerning optional coverage riders in private small employer plans and contracts. The state interpretation is that the most popular optional riders accompanying a specific benchmark product would be included as an essential health benefit, and by logical inference, less popular riders would not be covered and could simply be dropped without consequence from insurance products. Such a result willfully ignores the medical need for, and potential affordability of, less “popular” benefits, as well as any overall health policy reasons why a given benefit could be desirable as a cost-effective, privately-funded early intervention. The enshrining of optional riders that are popular at one point in time as a component of EHB may not reflect the needs and priorities of a changing, and aging population. It also defeats the purpose of having a large mandatory risk-sharing pool to overcome the individual human and social costs of adverse selection. These considerations may not naturally occur to professionals within the insurance industry, but are foremost in the understanding and experience of people with disabilities and disability advocates.
Once again, thank you again for informing the public and the disability community of the direction of HHS’s thoughts through the EHB Bulletin, and for extending the opportunity to comment on this critical issue for people with disabilities.
Sincerely,
Susan Henderson
Executive Director
Silvia Yee
Senior Staff Attorney
Endnotes
[1]Available at: Healthexchange.ca.gov (PDF)
[2]See for example the House floor statement of Congressman George Miller, Chairman of the House Education and Labor Committee upon passage of the ACA that the term rehabilitative and habilitative devices “includes durable medical equipment, prosthetics, orthotics, and related supplies.” [Congressional Record, H1882 (March 21, 2010)]
[3]Along with other disability and consumer advocates, DREDF submits that the EHB category of “rehabilitative and habilitative services and devices must encompass maintenance of function and the slowing of projected functional deterioration, and not only “restoration” of “normal” or prior functional abilities, and must also be interpreted broadly to include treatments and devices that enable individuals to live as independently as possible in the community, regardless of whether the underlying cause of impairment is disease, injury, or a chronic condition.
[4]The designation for Medicaid in California.
[5]California Medi-Cal defines DME as: serving a medical purpose, able to withstand repeated use, not useful to an individual in the absence of an illness, injury, functional impairment, or congenital abnormality, and appropriate for use in or out of the patient’s home.
[6]California’s Legislative Analyst’s Office, 2003-2004 analysis, reports that the state’s General Fund accounted for approximately $9.7 billion of Medi-Cal’s 2001-02 total expenditure of $26.5 billion. The California State Auditor (2002) reported that in 2001, Medi-Cal DME expenditures totaled $124.3 million (p.8).
[7]The growth rate of California’s DME expenditure in 2003 was 3.6%; this rate was lower than the overall state healthcare expenditure growth rate of 6.8%. Nationally, the U.S. Centers for Medicare and Medicaid Services also project that DME expenditures will decline as a percentage of national total healthcare expenditures (at www.healthguideusa.org).
[8]The Medi-Cal Policy Institute’s The California Working Disabled Program: Lessons Learned, Looking Ahead 2003 report states at p. 10 that “Nearly half (48 percent) of the disabled adults have private insurance and 25 percent are covered by Medi-Cal.”
[9]This estimate of 2.3%, or 326,000, is derived from responses to the 2003 California Health Interview Survey which asks respondents whether they have a health problem “that requires you to use special equipment such as a cane, a wheelchair, a special bed or a special telephone.”
[10]Available online at: http://www.chbrp.org/docs/index.php?action=read&bill_id=108&doc_type=3.
[11]California has a somewhat unique bifurcation of insurance. The California Department of Insurance (CDI) regulates health insurers that offer coverage for benefits to their enrollees through health insurance policies, while the Department of Managed Health Care (DMHC) regulates health care service plans that offer coverage for benefits to their enrollees through health care service plan contracts (e.g., managed care plans).
[12]The California Public Employees’ Retirement System (CalPERS) purchases and group purchases made by the Department of Health Care Services (DHCS) and Major Risk Medical Insurance Board (MRMIB), which act as group purchasers (respectively) for some Medi-Cal beneficiaries and for Healthy Family beneficiaries. CalPERS, Medi-Cal HMOs and Healthy Families all cover DME with no annual or lifetime benefit limit.
[13]The cost impact is greater in DMHC-regulated plans because they would have to transition from coinsurance to copayments to align DME coverage with coverage for other health care services and benefits which are typically expressed as a co-payment.
[14]Compare the snapshot of DME coverage in Disability Rights Education and Defense Fund California Health Insurance Plans–DME Coverage by 214 HealthPlans As of February 2007, available at: https://dredf.org/healthcare/CADME07_survey_update_mlb.pdf, to CHBRP 2010 report.
[15]Section 1302(b)(4)(B) states that the Secretary “must not make coverage decisions, determine reimbursement rates, establish incentive programs, or design benefits in ways that discriminate” based on certain factors. Section 1302(b)(4)(C) provides that essential items and services must not only be nominally covered but must “not be subject to denial to individuals against their wishes” based on certain factors.